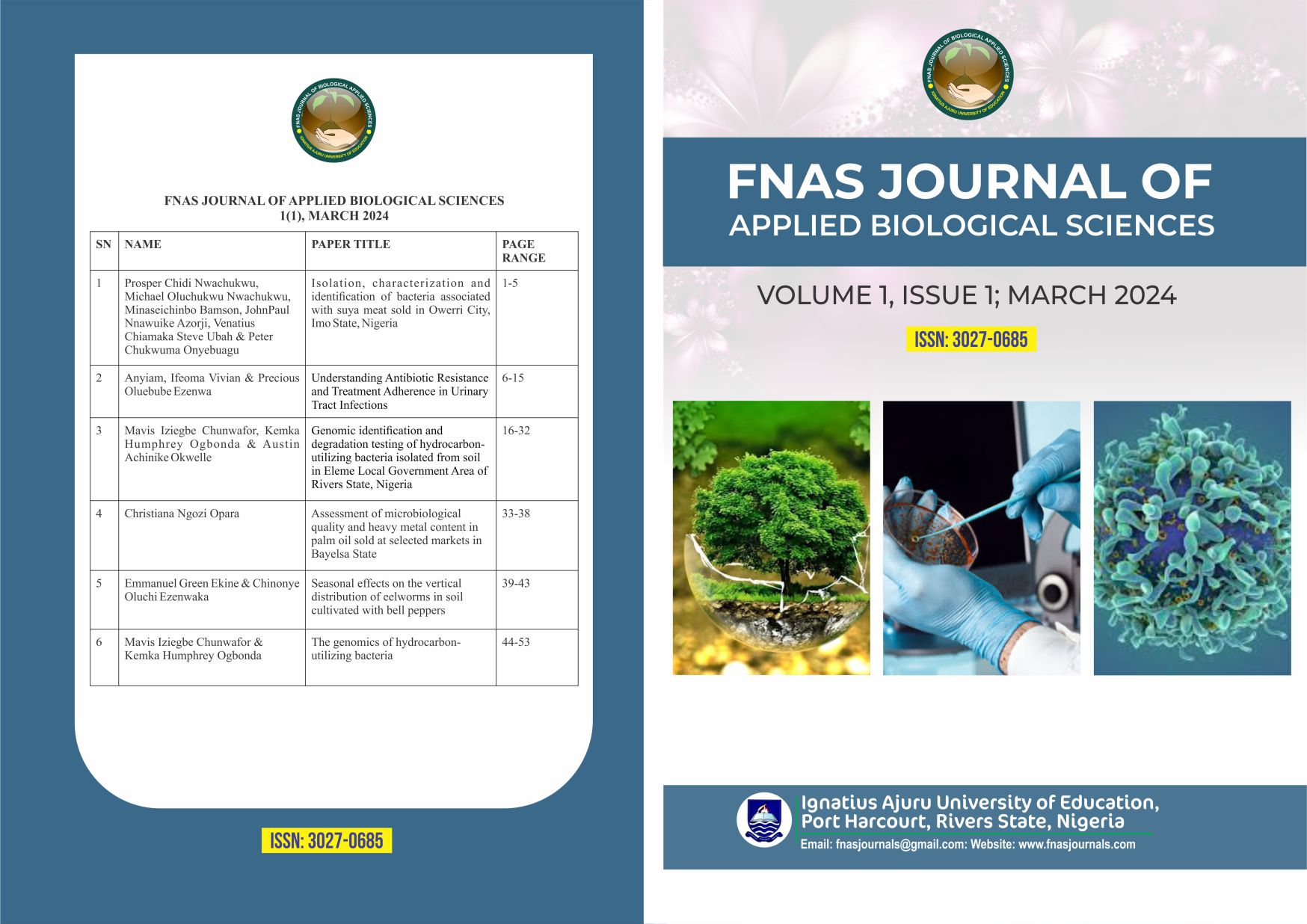
Understanding Antibiotic Resistance and Treatment Adherence in Urinary Tract Infections
Keywords:
Antimicrobial Resistance, Plasmid analysis, Biofilm formation, BacteriaAbstract
Microorganisms associated with urinary tract infection (UTI) can generate microbial biofilm, and this community of microorganisms can be produced by several bacteria that indicate antimicrobial resistance. One hundred mid-stream urine specimens from patients attending Federal Medical Center, (FMC) Yenagoa were examined to determine the antimicrobial resistance and biofilm formation of bacteria. Specimens were studied by culture and biochemical tests. The multidrug resistance pattern was determined using the standard agar disc diffusion method and plasmid profiling. The production of biofilm was assessed utilizing phenotypic techniques, specifically the Congo red agar method. The relationship between biofilm formation was analyzed using Pearson correlation test, and the antibiogram of the isolates. Results from this study revealed the presence of Citrobacter spp. 8(21%), Enterobacter spp. 5(13.1%), K. aerogenes 10(26.3%), P. mirabilis 6(15.7%), P. aeruginosa 5(13.1%), and S. aureus 4(10.5%). K. aerogenes 10(26.3%) was the predominant isolate, while the least was S. aureus 4(10.5%). The highest incidence of UTI was seen within age brackets 20-25 years with 17(44.7%) and 25- 30 years with 13(34.2%). Statistically, there was a significant difference between the age distribution (p< 0.05). In comparison, females had the highest number of bacterial isolates with 27(71%) while males with 11(28.9%). There was a significant difference in the percentage of occurrence of bacterial isolates. (p< 0.05). Most of the gram-negative bacterial isolates showed resistance to the various antibiotics. Citrobacter spp. and P. mirabilis were both susceptible to levofloxacin, ampiclox, nalixidic acid and tarivid. Enterobacter spp. showed resistance to all the antibiotics. K. aerogenes and P. aeruginosa were both susceptible to levofloxacin and tarivid. Staphylococcus aureus was resistant to cefuroxime, imipenem, cefotaxime, cefexime, gentamycin, ciprofloxacin, and amoxicillin but susceptible to levofloxacin, azithromycin, erythromycin, and tarivid. Biofilm formation was observed with Citrobacter spp. and P. mirabilis while there was no biofilm formation by Enterobacter spp. and S. aureus. The plasmid curing before and after plasmid curing indicated that most resistant antibiotics before curing were resistant except for tetracycline. After curing ciprofloxacin, gentamicin, chloramphenicol, tetracycline became sensitive to Citrobacter spp., Enterobacter spp., and P. mirabilis. The degree of antibiotic resistance to certain microbes is mostly influenced by misuse of drugs, therefore sensitization to antibiotic resistance should be a priority by physicians.