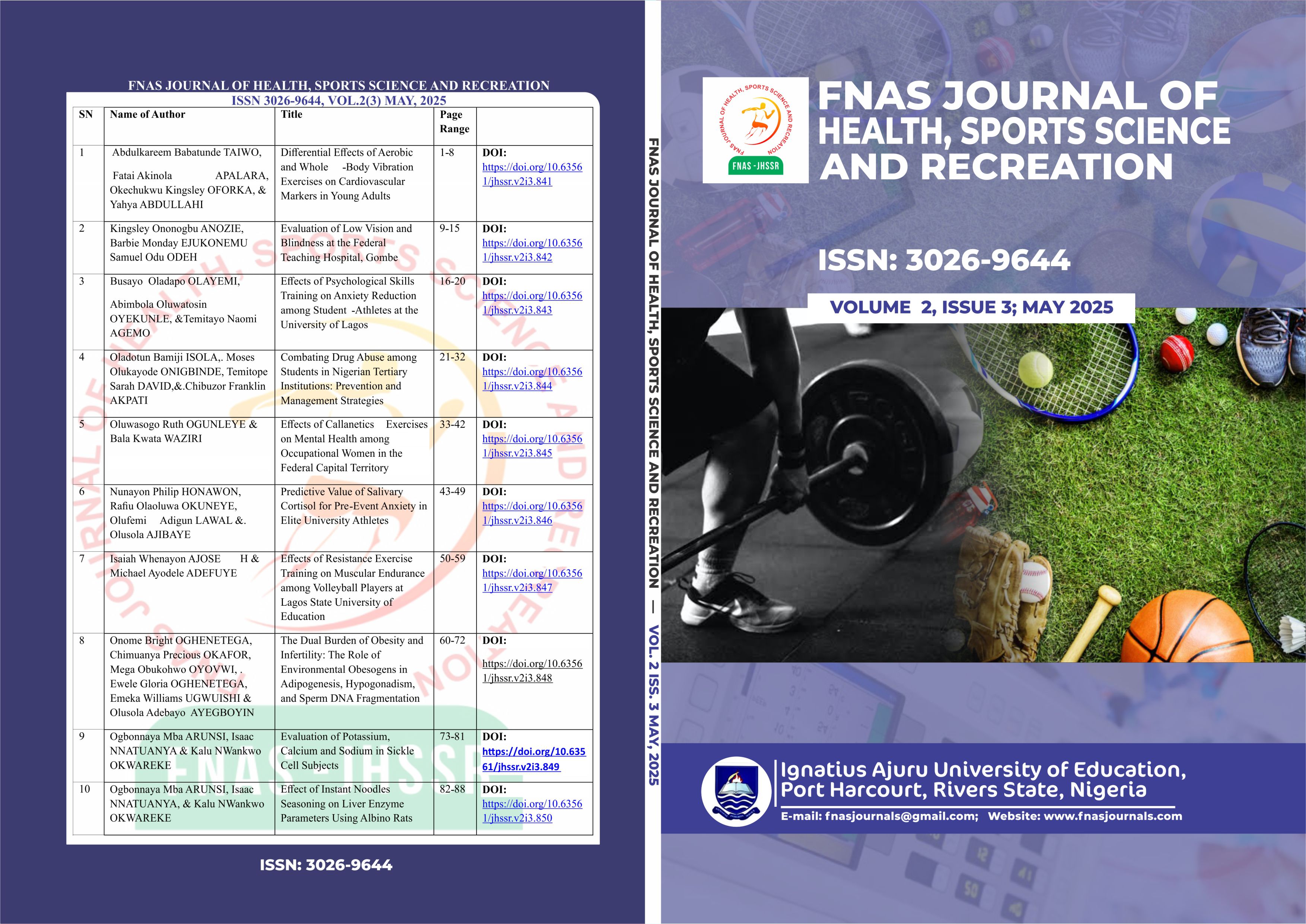
Evaluation of Potassium, Calcium and Sodium in Sickle Cell Subjects
DOI:
https://doi.org/10.63561/jhssr.v2i3.849Keywords:
Sickle cell, electrolyte imbalance, ion-selective electrode, hemolytic activity, HbSS and HbAA.Abstract
Electrolyte imbalances in SCD patients are frequently overlooked despite their significant role in disease progression and complications. This study aimed to evaluate serum electrolyte levels—potassium, calcium, and sodium—in sickle cell disease (SCD) patients and assess their clinical implications. This study was conducted at Madonna University Teaching Hospital in Nigeria, it employed a case-control design involving 132 participants, comprising 74 confirmed SCD patients (HbSS) and 58 age- and sex-matched healthy controls (HbAA). Blood samples were analyzed using an ion-selective electrode, revealing significant differences in electrolyte levels between groups. Specifically, SCD patients exhibit a markedly elevated serum calcium (4.98 ± 0.86 mmol/L) compared to controls (2.23 ± 0.23 mmol/L), with p < 0.001; higher sodium levels (152.29 ± 2.62 mmol/L) compared to controls (138.48 ± 3.68 mmol/L), with p < 0.001, and significantly lower potassium levels (3.28 ± 0.40 mmol/L) compared with controls (4.44 ± 0.66 mmol/L, with p < 0.001. These results shows that these alterations may result from chronic hemolysis, renal impairment, and metabolic stress associated with SCD, with elevated calcium possibly linked to bone resorption and hemolytic activity, while decreased potassium may occur as a result of cellular leakage and renal losses. Elevated sodium levels could reflect dehydration and impaired renal handling. These electrolyte disturbances are clinically relevant, as they predispose patients to arrhythmias, bone demineralization, and kidney dysfunction, thereby complicating disease management. The findings underscore the importance of routine electrolyte monitoring in SCD to detect early imbalances and implement targeted interventions. The study concludes that electrolyte disturbances are significant in SCD pathophysiology and recommends integrating regular electrolyte assessment into standard care, alongside nutritional counseling and patient education on hydration. Further research across diverse populations is warranted to validate these findings and elucidate underlying mechanisms, ultimately aiming to reduce morbidity and improve clinical outcomes in SCD patients.
References
Adebanjo, M. O., Adebayo, T. A., & Onyekwere, C. I. (2022). Calcium homeostasis in sickle cell disease: Implications for red blood cell stability. Hematology Research, 14(2): 189-204.
Adepoju, O. A., Akinola, N. O., & Ogunbiyi, T. M. (2022). Potassium ion transport and its therapeutic implications in sickle cell disease. Blood Reviews, 36(4): 65-72.
Adewoyin, A. S., Alagbe, A. E., & Awodu, O. A. (2015). Electrolyte and renal function profile during vaso-occlusive crisis in adult sickle cell anemia patients. Annals of Medical and Health Sciences Research, 5(6): 437–440.
Adeyemi, R. S., Osunlaja, A. O., & Bello, M. K. (2022). The role of dietary interventions in modulating calcium influx in sickle cell anemia. African Journal of Clinical Hematology, 10(3): 77-90.
Akinlade, K. S., Arogundade, F. A., & Adediran, A. (2011). Electrolyte and renal function in Nigerian sickle cell anemia patients. Nigerian Journal of Clinical Practice, 14(4): 418–421.
Almeida, F. T., Santos, B. R., & Souza, G. M. (2021). Electrolyte imbalance in sickle cell anemia: A key factor in disease pathophysiology. Hematology Reports, 13(2), 120-134.
Aygun, B., & Odame, I. (2012). A global perspective on sickle cell disease. Pediatric Blood & Cancer, 59(2): 386-390. DOI: https://doi.org/10.1002/pbc.24175
Ballas, S. K., Darbari, D. S., & Brugnara, C. (2018). Hematologic complications of sickle cell disease. Hematology/Oncology Clinics of North America, 32(2): 223-239.
Ballas, S. K., Gupta, K., & Adams-Graves, P. (2021). Sickle cell pain: A critical reappraisal. Blood, 137(21): 2878-2891.
Ballas, S. K., Gupta, K., & Adams-Graves, P. (2021). Sickle cell pain: A critical reappraisal. Blood, 136(20): 2371-2380.
Bartolucci, P., Brugnara, C., & Bogdanova, A. (2018). Ion transport and red blood cell dehydration in sickle cell disease. Haematologica, 103(10): 1563-1575.
Belcher, J. D., Nath, K. A., & Vercellotti, G. M. (2014). Vasculopathy in sickle cell disease: Evolving evidence of the role of oxidative stress and inflammation. American Journal of Hematology, 89(5): 497-502.
Bogdanova, A. Y., Makhro, A., & Kaestner, L. (2021). Dysregulated calcium transport in sickle cell disease and its impact on erythrocyte function. Blood Cells, Molecules, and Diseases, 89(1): 105-118.
Bogdanova, A., Makhro, A., Wang, J., Lutz, H., & Kaestner, L. (2020). Calcium in red blood cells—a perilous balance. International Journal of Molecular Sciences, 21(19): 7263.
Burtis, C.A, Ashwood, E.R, & Bruns, D.E. (2012). Electrolytes and blood gases. Tietz Textbook of Clinical Chemistry and Molecular Diagnostics 3(8): 29.
Dapaah, J. K., Badu, E., & Owusu, A. A. (2023). Potassium homeostasis and clinical manifestations in sickle cell patients. African Journal of Hematology, 15(1): 88-102.
Davies, S. C., Gilmore, A., Henthorn, J., & Brozovic, M. (2019). The role of infection in sickle cell disease. British Journal of Haematology, 73(4): 533-540.
de Franceschi, L., Cappellini, M. D., Olivieri, O., & Turrini, F. (2018). Modulation of erythrocyte ion transport in pathophysiology and treatment of sickle cell disease. Haematologica, 103(10): 1542-1552.
Dosunmu, T. O., Ajayi, R. A., & Olayemi, E. (2023). Pathophysiological mechanisms of ion transport in sickle cell disease. Journal of Medical Sciences, 11(3): 223-238.
Eldibany, M. M., & Totonchy, M. (2019). The sickle cell disease: Pathophysiology and management. The American Journal of Medicine, 132(6): 748-754.
Emokpae, M. A., Abhulimen, P. M., & Osime, U. (2009). Renal function and electrolyte levels in sickle cell anemia patients with proteinuria. Sierra Leone Journal of Biomedical Research, 1(1): 39–45.
Esrick, E. B., & Bauer, D. E. (2021). Genetic therapies for sickle cell disease. Seminars in Hematology, 58(2): 102-109.
Eze, I. C., Eze, D. O., & Nwangwu, K. C. (2012). Electrolyte changes in adult sickle cell anaemia patients in steady state. International Journal of Basic, Applied and Innovative Research, 1(4): 118–123.
Gibson, J. S., Muzyamba, M. C., & Cossins, A. R. (2021). Ion transport and the control of red blood cell volume: Pathophysiological perspectives in sickle cell disease. American Journal of Physiology-Cell Physiology, 320(2): C238–C250. DOI: https://doi.org/10.1152/ajpcell.00104.2005_COR
Gualandro, S. F., Pereira, B. B., & Mendes, A. L. (2022). The role of potassium transport abnormalities in sickle cell vaso-occlusion. International Journal of Hematology, 99(1): 56-68.
Hannemann, A., Rees, D. C., Brewin, J. N., Noe, A., Gibson, J. S., & Stewart, G. W. (2015). The Gardos channel: A key target for treatment of red cell dehydration in sickle cell disease. Blood, 125(22): 3422-3431.
Hines, P. C., Rankine-Mullings, A., & Reid, M. E. (2019). The effect of calcium channel blockers on sickle cell disease: A systematic review. Blood Advances, 3(16): 2404-2411.
Jensen, F. B., Rohde, S., & Brahm, J. (2019). Abnormal sodium transport in sickle cell disease: Mechanisms and therapeutic implications. Blood Cells, Molecules, and Diseases, 75(4): 112–121.
Joiner, C. H. (2018). Erythrocyte dehydration in sickle cell disease: Pathophysiology and therapeutic approaches. Blood Cells, Molecules, and Diseases, 69: 39-43.
Joiner, C. H. (2021). Sickle cell disease: Cellular and molecular pathophysiology. Blood Reviews, 42: 100711.
Makinde, A. M., Adigun, F. O., & Ogunleye, S. A. (2023). The Gardos channel and its role in sickle cell dehydration: A therapeutic target? International Journal of Hematology, 107(1): 99-114.
McGann, P. T., Ware, R. E., & Bendor, L. M. (2018). Sickle cell anemia in sub-Saharan Africa: Advancing the clinical paradigm through partnerships and research. Blood, 132(23): 2331-2336.
McGann, P. T., Ware, R. E., & Gordeuk, V. R. (2022). Renal complications and electrolyte imbalance in sickle cell anemia: Pathophysiology and management. Nature Reviews Nephrology, 18(6): 345–358.
Mendonça, R. A., Silva, L. P., & Barbosa, M. T. (2020). K-Cl cotransport dysfunction in sickle cell disease. European Journal of Hematology, 105(5): 329-345.
Mensah, E. O., Boateng, F. K., & Ofori, J. A. (2023). Plasma membrane calcium ATPase function in sickle cell disease: A potential target for therapeutic intervention. Clinical Hematology Journal, 12(2): 150-164.
Mishra, S., Patel, D. K., & Singh, A. K. (2023). Targeting ion transport mechanisms in sickle cell disease: Advances in therapeutic strategies. Frontiers in Physiology, 14: 1052317.
Nader, E., Skinner, S., Romana, M., Fort, R., Lemonne, N., Guillot, N., & Connes, P. (2021). Blood rheology: Key parameters in sickle cell disease. Frontiers in Physiology, 12: 630693.
Nduka, N., Iheonunekwu, N., & Okonkwo, M. (2013). Electrolyte disturbances in adult patients with sickle cell anemia. Tropical Journal of Medical Research, 17(2): 1–5.
Nwogoh, B., Adewoyin, A. S., Iheanacho, O. E., & Bazuaye, G. N. (2012). Prevalence of haemoglobin variants in Benin City, Nigeria. Annals of Biomedical Sciences, 11(2): 60-64.
Nzouakou, R., Ekou, A., & Kouadio, A. (2021). Hemolysis and electrolyte disturbance in sickle cell anemia: Clinical consequences. West African Medical Journal, 18(3): 175-189.
Okam, M. M., Mandell, E., & Sheehan, V. A. (2020). The role of sodium transport in sickle cell disease pathogenesis and treatment. Hematology/Oncology Clinics of North America, 34(5): 991–1006.
Okonkwo, I. R., Okonkwo, I. C., & Nwokediuko, S. C. (2014). Comparative study of plasma electrolytes and renal function in sickle cell anemia patients during crisis and steady states. Nigerian Journal of Clinical Practice, 17(4): 523–526.
Okonkwo, N. P., Alabi, A. T., & Ugochukwu, I. (2021). Combination therapy in sickle cell disease: The role of Gardos channel inhibitors and hydroxyurea. Journal of Sickle Cell Research, 15(1): 33-48.
Olayemi, E., & Bazuaye, G. N. (2010). Serum calcium, magnesium and phosphate levels in adult steady state sickle cell disease patients. Annals of African Medicine, 9(3), 158–161.
Piel, F. B., Steinberg, M. H., & Rees, D. C. (2017). Sickle cell disease. New England Journal of Medicine, 376(16): 1561-1573. DOI: https://doi.org/10.1056/NEJMra1510865
Quinn, C. T., Rogers, Z. R., & Buchanan, G. R. (2020). Survival of children with sickle cell disease. Blood, 115(4): 1316-1322.
Rees, D. C., Williams, T. N., & Gladwin, M. T. (2017). Sickle-cell disease. The Lancet, 376(9757), 2018-2031. DOI: https://doi.org/10.1016/S0140-6736(10)61029-X
Steinberg, M. H. (2011). Genetic etiologies for phenotypic diversity in sickle cell anemia. The Scientific World Journal, 11: 46-69. DOI: https://doi.org/10.1100/tsw.2009.10
Steinberg, M. H., Barton, F., Castro, O., Pegelow, C. H., Ballas, S. K., Kutlar, A., ... & Adams, R. J. (2015). Effect of hydroxyurea on mortality and morbidity in adult sickle cell anemia. JAMA, 289(13): 1645-1651. DOI: https://doi.org/10.1001/jama.289.13.1645
Stuart, M. J., & Nagel, R. L. (2020). Sickle-cell disease. The Lancet, 364(9442): 1343-1360. DOI: https://doi.org/10.1016/S0140-6736(04)17192-4
Tayo, B. O., Doumatey, A. P., Shriner, D., Huang, H., Ramos, E., & Adeyemo, A. (2015). Genetic architecture and gene–environment interactions in cardiovascular and metabolic disease in African Americans: The Jackson Heart Study. Current Cardiovascular Risk Reports, 9(3): 1–11.
Telen, M. J. (2020). Beyond hydroxyurea: New and old drugs in the pipeline for sickle cell disease. Blood, 127(7): 810-819. DOI: https://doi.org/10.1182/blood-2015-09-618553
Tiruneh, E. G., Teshome, A. A., & Assefa, A. Y. (2022). Disruption of calcium homeostasis in sickle cell anemia: Mechanisms and therapeutic implications. Ethiopian Journal of Hematology, 17(3): 200-215.
Tiruneh, T., Kassa, E., & Getachew, M. (2021). Calcium dysregulation in sickle cell disease: Implications for treatment. Journal of Hematology & Oncology, 14(1): 62.
Ware, R. E., de Montalembert, M., Tshilolo, L., & Abboud, M. R. (2017). Sickle cell disease. The Lancet, 390(10091): 311-323. DOI: https://doi.org/10.1016/S0140-6736(17)30193-9
Ware, R. E., Helms, R. W., & Elsherif, L. (2020). Genetic modifiers and the clinical heterogeneity of sickle cell disease. Pediatric Blood & Cancer, 67(2): e28045.
Zalawadiya, S., Siew, K. S., & Alex, A. B. (2021). Role of hydration in electrolyte balance and sickling episodes in sickle cell anemia. Journal of Hematology, 29(3): 289–300.